Colligo Academy Pocus Basics
Innehållsförteckning
Vascular Ultrasound
With the possible exception of pericardial tamponade, there is no other condition in which the rapid diagnostic capabilities of bedside sonography are of such striking benefit as abdominal aortic aneurysm (AAA). Emergency bedside ultrasonography enables the physician to confirm a high-risk diagnosis, decreasing the time needed to mobilize resources or even transfer the patent to a referral center if necessary. This one exam will save lives if incorporated into the regular practice of emergency and critical care physicians involved in the evaluation of acutely ill patients.
Manual of Emergency and Critical Care UltrasoundVicki Noble, 2011
Objectives
To reach the objectives for this module read the following text, watch the videos and finish the QUIZ.
- The ability to exam and identify the Aorta and understanding how pathological AAA can be diagnosed
- The ability to exam the lower extremities by 2-point compression protocol and by a more extended protocol
- Understanding the different ultrasound DVT exam protocols available by bedside and by radiology ultrasound
- Basic understanding of how to place peripheral IV lines and what factors increases success and survival rate of the IV line placed
1. Introduction
In this section we will learn to look at vascular structures of importance for emergency medicine. Starting with the aorta, continuing to DVT, before we finish with vascular access. With each section the difficulty increases, while the aorta is a relatively simple exam for our focused question: ‘is the aorta larger than 3cm?’, the section vascular access requires more practice and hand-eye coordination before basic proficiency is obtained.
And with vascular access there are certain procedures that are relatively easy to master, like securing an arterial line while intravenous access may prove to be much more challenging depending on the patients clinical and anatomical status.
2. Aorta
Aorta anatomy video (4.5min)
[Credit: Phillips Perera & SonoSite.]
Aorta pathology video (10min)
:
[Credit: Phillips Perera & SonoSite.]
When looking at the aorta the curvilinear probe is used and an abdomen protocol (the marker to the left of the screen). We start by putting the probe at a 90 degree angle against the patients abdomen, just below the xiphoid, with the marker pointing towards the patients right. In the image we should be able to identify the liver to the left side of the screen and a lumbar spine that casts shadow underneath it, and above the lumbar a pulsating round anechoic structure that is the aorta. The image depth should be optimized so that the aorta is in the center of the image with the lumbar on the lower edge of the image.
Once the aorta is identified and the image is optimized for depth (and gain), we can follow the aorta down to bifurcation that generally appears at the umbilical point. At the bifurcation the left and right iliac arteries should be followed for another couple centimeters, each respectively.
Once we looked at the aorta in short axis (out of plane view) the exam also includes looking at the aorta in long axis (in plane view). This is done by once again placing the probe below the xiphoid, identifying the aorta, and then rotating the probe in 90 degrees clockwise so that the marker is aimed at the patients head. Another way of obtaining the long axis view is by putting the probe with the marker aimed towards the patients head below the xiphoid, but slightly to the right side of the patient. As we swipe the probe slowly from right to left, and/or do a little bit of gentle fanning, we should acquire first the inferior vena cava and then the aorta.
A systematic review by Rubano et al from 2013 found that a pooled operating characteristics of emergency department ultrasound for the detection of AAA had a sensitivity of 99% and specificity of 98% (!) *.
3. DVT in Lower Extremities
DVT video (5 min):
Öppna video på vimeo.
(Denna video kan inte visas direkt utan måste ses på vimeo.)
[Credit: Jacob Avila & 5 min sono.]
The video above and the technique for evaluating lower extremities DVT in the emergency department by the emergency physician using POCUS, that has traditionally been taught, is a two-region compression (2-CUS) protocol. There is however certain disagreements concerning the validity and reliability of this protocol compared with more extensive protocols such as extended compression ultrasound (ECUS) and complete compression ultrasound (CCUS). See the image below, from a review by Needleman et al 2018*, for a good summary of the different protocols as they relate to the segments of the lower extremity veins examined:
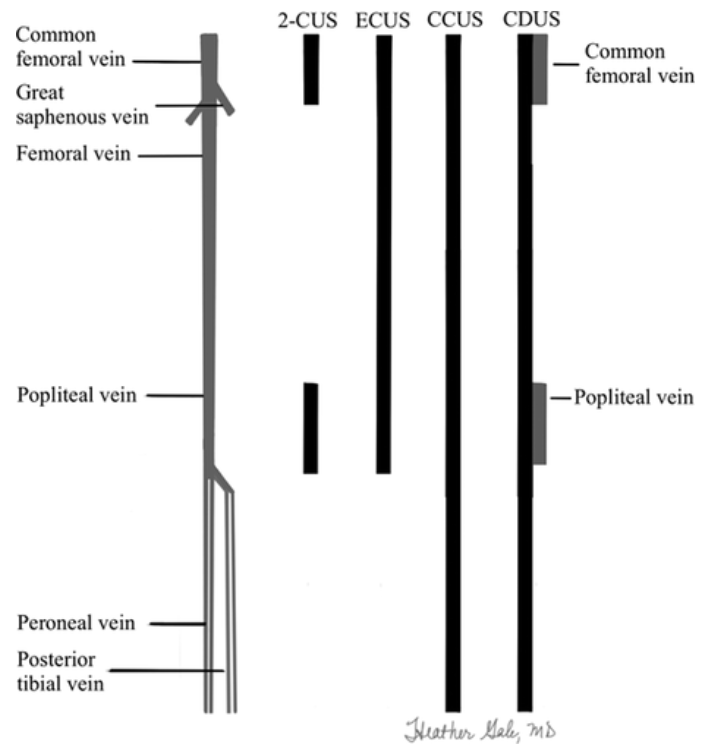
Figure 2 from Needleman et al, ‘Ultrasound for Lower Extremity Deep Venous Thrombosis: Multidisciplinary Recommendations From the Society of Radiologists in Ultrasound Consensus Conference’, 2018*.
Figure text: “Lower extremity venous system and extent of ultrasound tests. Black rectangles represent the extent of the compression ultrasound. Gray rectangles are sites of duplex Doppler. 2-CUS (2-region compression ultrasound) indicates compression ultrasound including the femoral veins 1 to 2 cm above and below the saphenofemoral junction and the popliteal veins up to the calf veins confluence; ECUS (extended compression ultrasound), the compression ultrasound from common femoral vein through the popliteal vein up to the calf veins confluence; CCUS (complete compression ultrasound), compression ultrasound from common femoral vein to the ankle; and CDUS (complete duplex ultrasound), compression ultrasound from the common femoral vein to the ankle (evaluating the posterior tibial and peroneal veins in the calf), color and spectral Doppler of the common femoral (or iliac veins) on both sides, color and spectral Doppler of the popliteal vein on the symptomatic side. Ultrasound of symptomatic areas may be required if the symptoms are not explained by the standard thigh-to-ankle examination.”
The image, and text, above is from the 2016 radiologist society consensus conference by Needleman et al*, where they recommend an ECUS examination to be performed in favor over a 2-region compression for bedside ultrasound physicians since, they argue, isolated femoral vein DVTs may be missed in a 2-CUS (when a CCUS exam can not be done by a radiologist in a timely matter). The video above by Jacob Avila recommends looking at least all the way down to mid-thigh, but also all the way to the knee if possible for the same reasons as the article by Needleman et al point out (making the videos examination a ECUS exam if the femoral vein can be visualised successful all the way down to the knee).
For the purposes of this course we’ve decided to teach both the 2-CUS and ECUS method, with the same caveat as the video mentioned: trying to visualize the femoral vein all the way from groin to the knee when possible (ECUS) but at least performing a 2-CUS when it proves difficult for the bedside examiner. The reasoning behind this approach is based on the clinical reality that: for the time being most of the clinics in Stockholm will still require an “official” examination by a trained radiologist to determine the diagnosis. So what is the benefit, if any, for bedside POCUS as it pertains to DVTs?
Well, as we mentioned previously POCUS is a part of all the other clinical tools you have at hand, such as: pretests (WELLs SCORE), D-dimer, and clinical context. For DVT we use bedside ultrasound to rule-in and never to rule-out a diagnosis. Even if you rule in a DVT the recommendation is still to have a radiologist perform an official examination too (unless you happen to work in a clinic where your images can be saved to the medical journals of the patient, where they can be cross-examined by trained ultrasound professionals for validation). The benefit of the bedside POCUS examination is first; during odd hours of the day (or in the ER) where a timely examination might not possible, and second; we recommend performing the examination even when a timely radiologist examination is available, since over time the practice will help you build a proficiency for evaluating DVTs.
Over time, our hope is, that this practice will evolve as will the local clinics ability to have a system for saving images to journals and having the necessary expertise for evaluating them, thus increasing the bedside reliability and validity of the exam.
2-point vs 3-point Compression Ultrasound
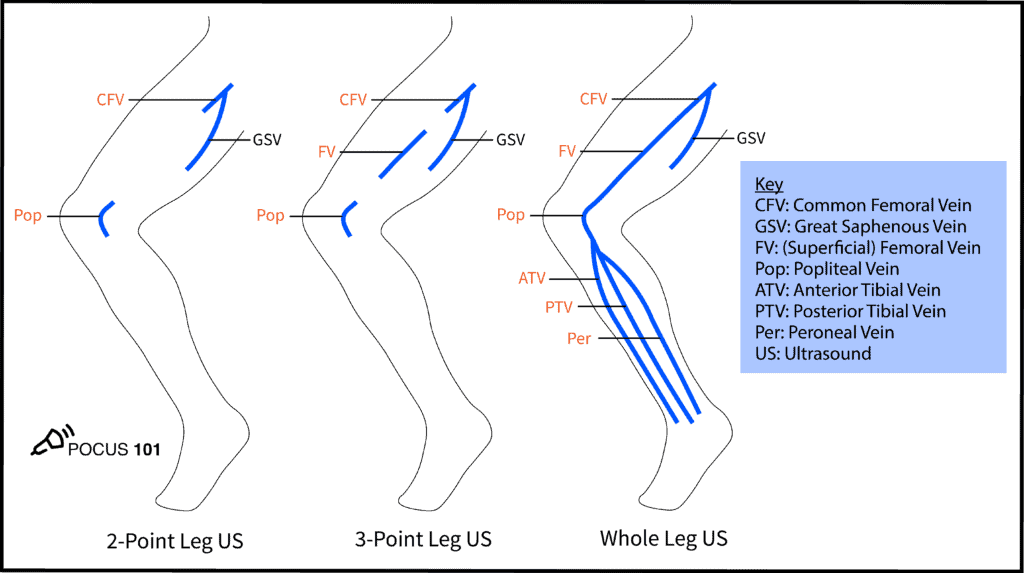
[Image credit: pocus101.com, DVT Ultrasound Made Easy: Step-By-Step Guide]
Having said that you should try to examen as far as between the groin and knee as you can, there is a meta study from 2019 that suggests that 2-point compression (2CUS) should be as reliable as a more extend examination (ECUS). The meta-analysis looked at 9 studies with 2-point compression (n=1337) where compressibility of femoral vein (CFV) and popliteal vein (PV) is examined and 8 studies with 3-point (n=1035) where the compressibility of CFV, superficial vein (SFV) and PV, as well as isolated SFV of lower extremity is examined. They found that “2-point POCUS (sensitivity: 91%, specificity: 98%) and 3-point POCUS (sensitivity: 90%, specificity: 95%) were excellent methods for the diagnosis of DVT. There was no significant difference in the diagnostic performance between the 2 methods. Moreover, the pooled proportions of the false-negative rate of the 2-point POCUS (4.0%) and 3-point POCUS (4.1%) were almost similar.”*
4. Vascular Access
Peripheral Venous Access Under Ultrasound Guidance – Part 1 (7 min):
Peripheral Venous Access Under Ultrasound Guidance – Part 2 (10 min):
For vascular access the probe of choice is the linear prove due to its high resolution for superficial structures. The marker on the probe should generally be aimed so that it corresponds with the screen, depending on which side of the patient you are standing. For our purposes it will most commonly be aimed towards the patients right with the marker on the screen being on the left side of the screen. When available an onscreen needle-guide can be used to help mark the middle of the image. As with all vascular access placements: preparation and good ergonomics is important for maximising your success rate. Sitting down next to the patients arm (if the access is to be placed there) with the ultrasound machine on the other side is a common set-up that works well in many cases. It is an advantage to have someone on the other side of the patient to help with changing settings on the ultrasound machine when necessary, such as gain and depth. It generally sufficient to use your judgement visually, and with compression, whether the vascular structure is an artery or a vein. Holding the probe with the non-dominant hand and the catheter/needle assembly with the dominant hand allows you to make the fine hand-momements needed.
There are two main techniques used for vascular access: the short axis (out-of-plane) and long axis (in-plane) view. The two views depend on individual preferences, and some practitioners prefer to switch between the two views during the procedure. The main advantage of the short-axis view is that relevant structures can be visualised, while the disadvantage is that the needle tip can be difficult to follow as it approaches the target structure.
For peripheral venous cannulation depth of <1,2 cm and a vein diameter of ≥ 4mm are associated with a higher success rate (and survival rate of the i.v. line) compared with smaller and shallower veins, as reported in one study with 151 patients from 2012 *. The same study concluded that vein depth is the biggest predictor of success both when it comes to success rate of cannulation and the survival of the i.v. line 48 hours after placement, resulting in placements in the antecubital fossa or forearm having improved survival compared to more proximal placement in deeper veins in the region of the brachial or basilic veins. The study, however, does not take into account i.v. line equipment such as “midline” that are constructed for more proximal and deep placements.
5. Summary
In this segment we covered the exams for aorta, DVT, and vascular access. The videos in the segment cover the practical part of the exam while the text, especially in the DVT section, is focused on different aspects of the reliability of the bedside exam.
6. Pitfalls
Aorta
- Use compression to displace bowel gas if you’re having difficulty when visualizing the aorta.
- Remember to measure the entire vessel not just the lumen as abdominal aortic aneurysms often have mural thrombus.
- Not mistaking the IVC for the aorta: the latter is on the patients left, has a thicker and more echogenic wall, and is round in short-axis while the IVC is often teardrop shaped.
- Remember to visualize the entire aorta, from the diaphragm to bifurcation to exclude the presence of an aneurysm
- Rule in do not rule out! This is especially true for the diagnosis of aortic dissection, while a dissection flap can sometimes be visualized and should then be followed up promptly, a failure to visualize a flap by ultrasound does not exclude aortic dissection.
- For the iliace arteries the cut-off taught at POCUS courses is 1,5 cm, however from a radiology perspective a iliaca artery of 1,5-2,0/2,5 is considered ectactic and above 2 or 2,5 (depending on local guidelines) is considered aneurysmal – but an ectactic iliaca artery needs follow up too, contact the vascular surgeons when unsure!
DVT
- Use the curvilinear probe if you can’t visualize the deep veins when examining a larger patient
- If your having problems visualizing the popliteal vein: try having the patient hang the legs over the edge of the bed to distend the vessels
- Lymph nodes may mimic a thrombus, be sure to scan through the entire structure as a lymph node will appear discrete and separate from vessels
- To fully evaluate the common femoral vein, make sure to visualize the proximal region at the confluence of the greater saphenous and common femoral veins
Vascular Access
- Avoid, if possible, peripheral line in vessels less than 4mm in diameter or that are deeper than 14 mm from the skin.
- Proximal veins have a higher survival rate after 24 hours than more distal ones.
- Practice without ultrasound too so you learn the hand mechanics needed and can focus on the screen without worrying too much about your hand movement.
7. Quiz
8. Further Reading
Books
-
- Noble. ‘Manual of Emergency and Critical Care Ultrasound’. 2nd Edition. 2011.
- ch. 5 Abdominal Aorta Ultrasound
- ch. 8 Ultrasound of the Deep Venous System
- ch. 15 Vascular Access
- Dawson & Mallin. ‘Introduction to Bedside Ultrasound – Vol 1’. 2013.
- ch. 3 Aorta
- Dawson & Mallin. ‘Introduction to Bedside Ultrasound – Vol 2’. 2013.
- ch. 8 Peripheral IV Placement
- ch. 12 DVT
- Soni et al. ‘Point-of-Care-Ultrasound’. 2nd Edition. 2020
- ch. 28 Abdominal Aorta
- ch. 34 Lower Extremity Deep Venous Thrombosis
- ch. 37 Peripheral Venous Access
- ch. 38 Arterial Access
- Noble. ‘Manual of Emergency and Critical Care Ultrasound’. 2nd Edition. 2011.
9. References
Aorta
- Bentz et al. ‘Accuracy of emergency department ultrasound scanning in detecting abdominal aortic aneurysm’. 2006
- Rubano et al. ‘Systematic review: emergency department bedside ultrasonography for diagnosing suspected abdominal aortic aneurysm’. 2013.
DVT
- Needleman et al. ‘Ultrasound for Lower Extremity Deep Venous Thrombosis: Multidisciplinary Recommendations From the Society of Radiologists in Ultrasound Consensus Conference’. 2018.
- Zitek et al. ‘Mistakes and Pitfalls Associated with Two-Point Compression Ultrasound for Deep Vein Thrombosis’. 2016
Vascular Access
- Beecham et al. ‘Peripheral Line Placement’. 2019
- Fields et al. ‘The effect of vessel depth, diameter, and location on ultrasound-guided peripheral intravenous catheter longevity’. 2012.
- Stolz et al. ‘Ultrasound-guided peripheral venous access: a meta-analysis and systematic review’. 2015.
- Weiner et al. ‘Ultrasound-guided vascular access: a comprehensive review’. 2012
[Version 2.0 — Last updated 2022-07-01 — Status: Active]
[Version 2.0, update 2022-07-01: added subsection “2-point vs 3-point Compression Ultrasound” to 3. DVT. Moved quiz from google docs to in-page.]


