Colligo Academy Pocus Basics
Innehållsförteckning
Ultrasound in Clinic
What we weren't sure about in 2007 was whether medicine would recognize and embrace the potential that we saw in ultrasound technology. This is now happening, and quickly. Ultrasound education is now part of emergency medicine, critical care, and surgical training programs. Several medical schools in the United States are longitudinally integrating ultrasound into their curriculum - both in the preclinical (anatomy, pathophysiology) and clinical years.
Manual of Emergency and Critical Care UltrasoundVicki Noble, 2011
Our study suggests that bedside emergency ultrasound (EUS) can increase patient satisfaction. In light of increasing hospital and health care organization emphasis on satisfaction metrics, there is more reason than ever to utilize bedside EUS. As more health care organizations and hospitals emphasize satisfaction surveys, the argument in favor of emergency physicians ultrasound performance becomes stronger, not just to expedite care and improve care and diagnosis, but also as a simple tool to maximize satisfaction scores and improve the patient–physician relationship.
Bedside ultrasound maximizes patient satisfactionHoward et a, 2014
Objectives
There is no QUIZ and no videos for this module. Only my thoughts on how to use bedside ultrasound in-clinic, how to improve on a personal level, how to create an ultrasound community in your local hospital, what structural improvements that are needed, and finally a few thoughts on progression and ethics.
1. Introduction
This segment is some thoughts and considerations on how to use ultrasound in clinic after this course is over. The students of this course will be doing their residency in hospitals at many different locations in Sweden. While we acknowledge that bedside ultrasound integration, equipment, and routines will vary to a huge degree depending on the size and traditions of each hospitals, I have composed some thoughts on achieving local improvement and on best practices.
You will notice throughout this course that each and every one of us instructors are very enthusiastic about using and teaching ultrasound, and my hope is that you will feel the same way and use the knowledge you’ve gained during this course on a daily basis and, also, to pass the knowledge on to other fellow clinicians.
2. Stickiness:
Daily Bedside Ultrasound Practice
In the beginning nothing will substitute improvement in bedside ultrasound proficiency more than getting a lot of practice on patients with and without pathology. From our experience the residents that continue practicing with the ultrasound machine and use it on a daily basis will improve the most over time.
Having said that, having access to experienced ultrasound teachers and doing proctored bedside ultrasound exams when possible is a key component too (more on that below). However, we know that that may not always be possible due to the lack of preexisting structures for new bedside ultrasound practitioners in many clinics outside Stockholm at the present moment.
We’re also fully aware of the high-stress nature of many emergency clinics where many clinicians feel like they don’t have the time to start the ultrasound machine and perform an exam on each patient. Especially if the clinicians are planning a CT-scan, chest X-ray or an ultrasound by radiologists, they may reason that there is no point of doing a bedside ultrasound exam too. I would like to make the argument that those cases are excellent opportunity for learning as you will get an “official” adjunct to compare your ultrasound findings with.
Bedside ultrasound does not need to take more than a couple minutes of your time (and in the case of FAST shouldn’t), and in the beginning my advice would be to do it (almost) as often as you use your stethoscope to listen to the heart and lungs. If for no specific focused question, then just for the benefit to get a visualized image of the lungs to help you create a memory bank of healthy and pathological LUS images.
My standard introduction before using the ultrasound when examining each patients is:
“I’m going to look with ultrasound on [insert specific area of focus], but before I do I just want to tell you that I am not a radiologists or cardiologist. This is not an official exam and I can’t evaluate the images as well as the radiologists can. However I can, sometimes, evaluate certain findings that can help in my assessment as an emergency physician. You will get a little sticky and cold from the ultrasound gel but it is colourless and will wash off. I hope that is ok?”
I recommend for you to create a similar introductory phrase that you say when examining each patient, so they don’t leave the emergency clinic or the ward thinking they have done an official ultrasound of the heart, kidneys, or whatever organ that you’ve evaluated with focused questions.
Besides all the benefits of ultrasound improving clinical decision making and diagnosis and, sometimes, saving the patient radiation it also makes the patients more satisfied with the hospital visit. A study from Howard et al published 2014 found that patients who had a bedside ultrasound exam had statistically significant higher satisfaction scores with overall ED care, diagnostic testing, and with their perception of the physician *. This finding is, I would argue, kind of a big deal and should not be understated. My experience performing bedside ultrasound in the ER for the past 5 years is similar to the findings from the study. The bedside ultrasound exam will help you make a better connection with the patient and that is always important for overall clinical accuracy, compliance, and, in short, for providing good care.
3. Quality & Validation part 1:
Creating a Bedside Ultrasound Community
Ensuring the quality of exams performed by physicians learning bedside ultrasound requires access to competence that can evaluate each, or at least, a set of number of exams for each organ/protocol and provide relevant feedback. As proctored exams are not always available, saving images and having them reviewed by a competent practitioner later is one solution to the lack of proctored exams that we have implemented in our emergency hospital.
At our clinic, each POCUS trainee is required to do a certain number of exams of each organ/protocol mentioned with a certain number of pathologies identified before they can obtain their “beside-ultrasound-license” and write their findings in the patient journal (with strict rules of what they can and can’t assess/write). In the best of worlds the images are stored too, in a central journaling system, where others in the hospital (including radiologists) can see and evaluate them. More on that below.
My suggestion for those of you doing their residency in smaller hospitals where there is not enough bedside ultrasound expertise, knowledge, or resources in your clinic for a structured POCUS curriculum to start building your own POCUS community.
Make an inventory of interested participants both from your clinic but also from the radiologists, cardiologists, and biomedical analysts that are proficient in ultrasound exams, and interested in helping, in each of their respective fields. Also you could create a What’sApp or Signal messaging group where you can discuss ultrasound (however be careful with sensitive patient data/images).
4. Quality & Validation part 2:
Journaling and Documentation
In the best of worlds your clinic will embrace bedside ultrasound and value it and its benefits by investing in a journaling-solution where images can be stored and reviewed similar to how images are stored in SECTRA at the moment.
This is the big key to any bedside ultrasound practice in any clinic and will not only be the biggest game changer, but an absolute requirement, when going forward towards improving the validity and reliability of bedside ultrasound in Swedish hospitals. The proof is, as they say, in the pudding and having ultrasound clips stored and accessible in patients journals will help others (radiologists, cardiologists, emergency physicians, etc) to review and assess if what the POCUS practitioner claim in the journal is a correct assessment or not. It will also help push the boundaries between bedside and non-bedside ultrasound as each clinic, and each physician, progresses.
5. Teaching Bedside Ultrasound: Passing on the Knowledge
We are of the firm belief that bedside ultrasound improves physicians clinical assessment and should be thought and practiced even without, or in the period until, the journaling & teaching structures mentioned above is implemented.
To help spread bedside ultrasound knowledge, my best advice is to differentiate between who can teach and who can validate the quality of the exam and the findings. Anyone can learn and teach bedside ultrasound, however each clinic has to decide who can assess what and what is required to become the bedside “expertize” at each clinic judging the accuracy of the exams. At least until (if) a national consensus is created. One of our aims with this course is to get the conversation going regarding what should and should not be included in a POCUS course and what qualifies trainees and, in extension, POCUS teachers.
6. Progression of Bedside Ultrasound:
Levels of Competence
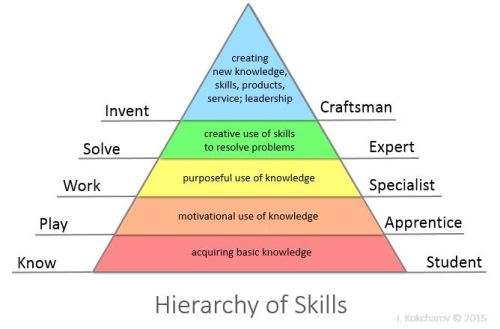
[Image credit: Kokcharov]
As bedside ultrasound progresses, we have a suggestion for the levels of competence to strive for:
Level 1 – individual
- Basic POCUS knowledge after a course like or similar to this one. The POCUS practitioner can not yet write their evaluation in journals, but can use bedside ultrasound in clinic and save images for review of someone who is “authorized” to evaluate them.
Level 2 – individual
- The POCUS practitioner has completed a number of reviewed or proctored exams of each module with a certain amount of these being pathological. A more competent teacher evaluates the exams for picture quality and correct assessment(s) before the student is “licensed/auhtorized” to document their assessment in patient journals.
Level 3 – individual and system
- POCUS becomes standardized with national consensus, and the requirements for each level becomes similar to the ATLS-course or CPR-course with clear requirements for students and teachers certificates.
Level 4 – individual and system
- The POCUS practitioner can, after the steps above, also save the image to a central journaling system. A percentage of images saved are randomly and regularly reviewed by experts for quality and validity control.
Level 5 – individual and system
- The POCUS practitioner does 3-6 month rotations with radiologists and echocardiographers respectively, qualifying the practitioner to make assessments considered beyond the scope of bedside ultrasound.
Level 6 – research
- Do research on best practices for POCUS! Design smart new studies and figure out important metrics for evaluating POCUS training and applications. Replicate and retest previous studies. Participate in the local, national, and global conversation of what POCUS brings to the clinical table and how it can evolve (also se image above: i.e. craftsman).
NOTE: This is not an absolute roadmap for the progression of bedside ultrasound in each clinic, but mostly food for thought and something to work on in a longer timespan. Note that level 3, a national consensus, is not mandatory for the other steps as such an endeavour might take too long if it happens at all, due to several factors, compared to the other levels that can, in principle, be implemented rapidly and (in practice and principle) simultaneously all at once.
7. Ethics
Finally a few words on ethics. Be humble, in the beginning most of your exams in clinic should just be teaching opportunities. If you find something suspicious looking that you cant evaluate but that doesn’t need urgent attention (such as a big kidney cyst or a suspect looking liver) ask a more competent colleague for help when available, and when not use your clinical judgement and provide for appropriate, and timely, clinical follow-up (by referring to official radiology or primary health care follow-up). Make sure the non-critical patient is comfortable with the exam and abstain from doing the exam if they are not and if you judge that it’s not necessary. Most patients, as mentioned above, will not only be ok with ultrasound exams when asked politely but might find the in-hospital experience better because of it.
8. Further Reading & References
Books
- Noble. ‘Manual of Emergency and Critical Care Ultrasound’. 2nd Edition. 2011.
- No relevant chapters for this module.
- Dawson & Mallin. ‘Introduction to Bedside Ultrasound – Vol 2’. 2013.
- Ch. 19 Administration
- Soni et al. ‘Point-of-Care-Ultrasound’. 2nd Edition. 2020
- Ch. 49 Competence, Credentialing and Certification
References
- Howard et al. ‘Bedside ultrasound maximizes patient satisfaction’. 2014.
[Version 2.0 — Last updated 2022-07-01 — Status: Active]
[Version 2.0, update 2022-07-01: minor revisions/spell-checks.]


